Kidney pain shouldn’t be ignored as it may signal serious conditions like kidney stones, UTIs, kidney infections, polycystic kidney disease, glomerulonephritis, hydronephrosis, renal vein thrombosis, kidney cancer, kidney trauma, or renal abscesses. You’ll feel most kidney pain in your flank area (sides and back) and it often comes with other symptoms like fever, urination changes, or blood in urine. Understanding these common causes can help you seek timely medical attention and prevent complications.
Key Takeaways
- Kidney stones cause excruciating pain and require immediate attention, especially when accompanied by fever, nausea, or blood in urine.
- Urinary tract infections that ascend to kidneys (pyelonephritis) cause flank pain, high fever, and require prompt antibiotic treatment.
- Polycystic kidney disease leads to flank pain, high blood pressure, and blood in urine due to fluid-filled cysts.
- Kidney trauma from accidents or contact sports can cause internal bleeding hours after injury and needs immediate medical care.
- Hydronephrosis, where urine backs up into kidneys, causes progressive pain and can lead to permanent kidney damage if untreated.
Kidney Stones: When Minerals Crystallize and Cause Pain

Kidney stones rank among the most excruciating causes of kidney pain, often described by sufferers as worse than childbirth. These hard mineral deposits form when substances in your urine concentrate and crystallize.
When they move through your urinary tract, they can trigger intense, stabbing pain that typically radiates from your side and back to your lower abdomen and groin.
Your dietary factors play a significant role in stone formation. Foods high in oxalate, sodium, and animal protein increase your risk, while calcium-rich foods—contrary to popular belief—may actually help prevent stones.
Your hydration levels are equally essential; insufficient water intake concentrates urine, creating an ideal environment for crystal formation.
Most doctors recommend drinking enough water to produce at least 2 liters of urine daily to flush potential stone-forming minerals from your system.
Urinary Tract Infections That Spread to the Kidneys
While most urinary tract infections (UTIs) remain confined to the bladder, untreated infections can ascend through the ureters to reach your kidneys, causing a serious condition called pyelonephritis.
When a UTI reaches your kidneys, you’ll notice more severe symptoms than typical urinary symptoms. These include high fever, flank pain, nausea, and sometimes confusion. Immediate medical attention is necessary to prevent complications like kidney damage or sepsis.
| Symptom | Bladder UTI | Kidney Infection |
| Pain | Lower abdomen | Flank/back pain |
| Fever | Mild or none | High (≥101°F) |
| Urination | Burning, frequency | Painful, urgent |
| Appearance | Cloudy urine | Blood in urine |
| Severity | Uncomfortable | Potentially dangerous |
Infection prevention includes staying hydrated, urinating after intercourse, and completing prescribed antibiotics.
Polycystic Kidney Disease: When Cysts Multiply
Unlike most kidney conditions that develop from external factors, polycystic kidney disease (PKD) is an inherited genetic disorder characterized by the growth of numerous fluid-filled cysts in both kidneys.
As these cysts develop and grow, they cause cystic enlargement of your kidneys, sometimes expanding them to several times their normal size. This expansion creates pressure on surrounding tissues, resulting in flank pain, back discomfort, and abdominal fullness.
You may experience blood in your urine, high blood pressure, and urinary tract infections more frequently.
PKD runs in families, with genetic factors determining whether you’ll develop the condition. There are two main types: autosomal dominant PKD (more common, appearing in adulthood) and autosomal recessive PKD (rarer, affecting infants and children).
Kidney Infections (Pyelonephritis): More Serious Than You Think
When bacteria invade your upper urinary tract, they can trigger pyelonephritis, a potentially severe infection that rapidly turns dangerous if left untreated.
Unlike simple UTIs, kidney infections cause intense flank pain, high fever, chills, and sometimes nausea and vomiting.
You’ll need antibiotics immediately, typically for 7-14 days. In severe cases, hospitalization for IV medications may be necessary.
Don’t delay seeking care—untreated infections can cause permanent kidney damage or sepsis.
Some people develop chronic symptoms after repeated infections, including persistent discomfort and recurring episodes.
Treatment options expand beyond antibiotics to include addressing underlying causes like structural abnormalities or kidney stones.
If you experience fever with back pain, especially with urinary changes, contact your doctor right away.
Glomerulonephritis: Inflammation of the Kidney’s Filtering System
Glomerulonephritis affects your kidneys’ filtering units, often causing symptoms like blood in urine, swelling in your face or legs, and unusual fatigue that you shouldn’t ignore.
Your doctor will likely order urinalysis, blood tests, and possibly a kidney biopsy to confirm the diagnosis and determine the underlying cause.
Treatment typically includes medications to reduce inflammation, managing blood pressure, and sometimes immunosuppressive drugs, with most patients experiencing significant improvement within weeks to months of starting appropriate therapy.
Symptoms to Watch For
The inflammatory condition affecting your kidney’s filtration units presents with several recognizable warning signs.
You’ll often notice pink or cola-colored urine, indicating blood presence. Foamy urine suggests protein leakage, while facial puffiness, especially around your eyes, signals fluid retention.
Watch for swelling in your ankles and feet that worsens throughout the day—a vital indicator for kidney health assessment.
You might experience fatigue, nausea, and reduced urination as your kidneys struggle to filter properly. Some patients report dull, persistent flank pain that requires appropriate pain management.
If you’re experiencing high blood pressure resistant to medication or unexplained shortness of breath, consult your doctor immediately.
Early detection greatly improves treatment outcomes for glomerulonephritis and prevents permanent kidney damage.
Diagnosis and Testing
Diagnosing glomerulonephritis typically begins with a thorough evaluation of your symptoms, medical history, and risk factors. Your doctor will order several tests to confirm the condition and determine its severity.
| Test Type | Purpose | What to Expect |
| Urinalysis results | Detect protein, blood, or inflammatory cells | You’ll provide a urine sample for laboratory analysis |
| Blood tests | Measure kidney function, identify infections | Simple blood draw to check creatinine and BUN levels |
| Imaging studies | Visualize kidney structure and size | Ultrasound or CT scan to examine kidney appearance |
A kidney biopsy may be necessary in some cases to examine tissue samples under a microscope. This procedure helps determine the exact type of glomerulonephritis you have and guides your treatment plan. Early diagnosis greatly improves your chances of successful treatment.
Treatment and Recovery
Once diagnosed, treating glomerulonephritis requires a personalized approach based on the underlying cause and severity of your condition.
Your doctor may prescribe corticosteroids to reduce inflammation or immunosuppressants to prevent your immune system from attacking kidney tissues.
For mild cases, you’ll need to make specific lifestyle changes to support kidney healing.
These include limiting salt intake, managing blood pressure, and staying adequately hydrated.
Dietary adjustments are essential—you should reduce protein consumption and avoid foods high in potassium if your kidneys aren’t filtering properly.
Recovery timelines vary considerably.
Acute cases may resolve within weeks with proper treatment, while chronic glomerulonephritis requires ongoing management.
Throughout recovery, you’ll need regular bloodwork and urine tests to monitor kidney function and guarantee your treatment plan remains effective.
Kidney Trauma From Accidents or Impact Injuries
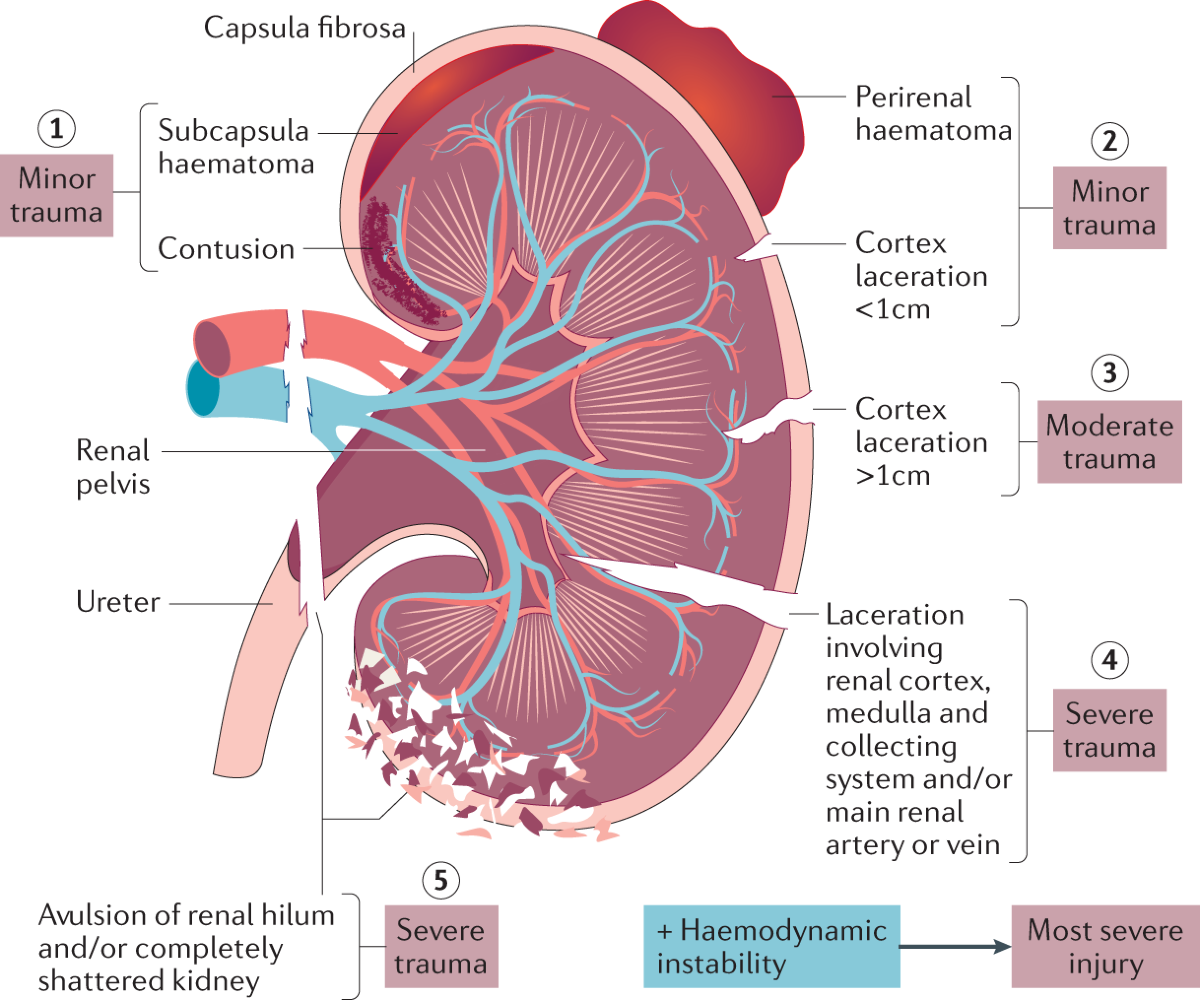
Physical impacts to your back or abdomen can result in potentially serious kidney injuries that shouldn’t be overlooked. Your kidneys are partially protected by your lower ribs, but direct blows from car accidents, sports collisions, or falls can cause bruising, bleeding, or even ruptures.
Watch for symptoms like intense flank pain, blood in urine, nausea, and bruising across your back. Immediate impact assessment by medical professionals is vital—even if you feel “fine” initially, internal bleeding can develop hours later.
Don’t underestimate kidney protection during high-risk activities. Wear appropriate gear for contact sports and proper seatbelts while driving.
If you’ve experienced any considerable trauma to your back area, don’t wait for symptoms to worsen before seeking emergency care. Prompt treatment greatly improves outcomes for kidney trauma.
Hydronephrosis: When Urine Backs up Into Your Kidneys
While many kidney conditions develop gradually, hydronephrosis creates pain through a more mechanical process—urine backing up into your kidneys when it can’t drain properly. This urine retention causes kidney swelling, leading to pain that ranges from dull to severe.
| Hydronephrosis | Symptoms | Treatment Options |
| Mild | Subtle flank pain, occasional discomfort | Monitoring, treating underlying cause |
| Moderate | Persistent pain, urinary changes | Medications, stent placement |
| Severe | Intense pain, nausea, fever | Surgical intervention, nephrostomy tube |
You’ll typically experience worsening symptoms as blockages persist. Common causes include kidney stones, tumors, and enlarged prostate in men. Don’t ignore these symptoms—untreated hydronephrosis can lead to permanent kidney damage. Your doctor will use imaging tests like ultrasound to confirm diagnosis and determine the appropriate treatment path.
Renal Vein Thrombosis: Blood Clots in Kidney Veins
When blood clots form in the veins that drain your kidneys, a serious condition called renal vein thrombosis (RVT) develops. This venous obstruction prevents blood from properly leaving your kidney, causing swelling, reduced kidney function, and often significant pain.
You’re at higher risk for RVT if you have nephrotic syndrome, cancer, severe dehydration, or a blood clotting disorder. Women taking certain hormonal medications may also face increased risk of clot formation.
Symptoms typically include severe flank pain, blood in urine, and decreased urination. In some cases, you’ll develop fever and high blood pressure.
Early diagnosis is vital as RVT can lead to permanent kidney damage. Your doctor will likely use imaging tests like CT scans or ultrasounds to confirm the diagnosis before starting treatment.
Kidney Cancer: Understanding the Warning Signs
Kidney cancer often develops silently in its early stages, making it crucial to recognize potential warning signs before the disease progresses.
When symptoms do appear, you might notice blood in your urine, persistent pain in your side or back, a lump in your abdomen, unexplained weight loss, or chronic fatigue.
Early detection greatly improves treatment outcomes. If you’re experiencing these symptoms, especially with risk factors like smoking, obesity, high blood pressure, or family history of kidney cancer, consult your doctor promptly.
Men over 50 face higher risks, but kidney cancer can affect anyone.
Don’t dismiss persistent side pain as merely muscle strain. While most kidney pain stems from less serious conditions, recognizing cancer symptoms guarantees you receive timely medical intervention when necessary.
Kidney Abscesses: Pockets of Infection in Renal Tissue
A less common but severely painful kidney condition emerges when bacteria infiltrate and multiply within renal tissue, creating kidney abscesses. These pockets of pus typically develop when an existing urinary tract infection spreads to your kidneys and remains untreated.
You’ll recognize abscess formation through persistent high fever, intense flank pain, chills, and profound fatigue. These infection symptoms often appear more severe than typical kidney infections and don’t respond to standard antibiotics.
You might also experience nausea, vomiting, and changes in your urination patterns.
Don’t delay seeking medical attention if you suspect a kidney abscess. Treatment typically requires specialized antibiotics and possibly drainage procedures.
Without proper intervention, the infection can spread to your bloodstream, leading to sepsis – a potentially life-threatening complication requiring immediate emergency care.
Conclusion
Your kidneys are essential filtration powerhouses that need your attention. If you’re experiencing persistent flank pain, don’t wait to see a doctor. Early intervention can prevent serious complications and preserve kidney function. Did you know that 1 in 10 people worldwide have chronic kidney disease, yet 90% don’t know they have it? Listen to your body’s warnings—your kidneys are too significant to ignore.